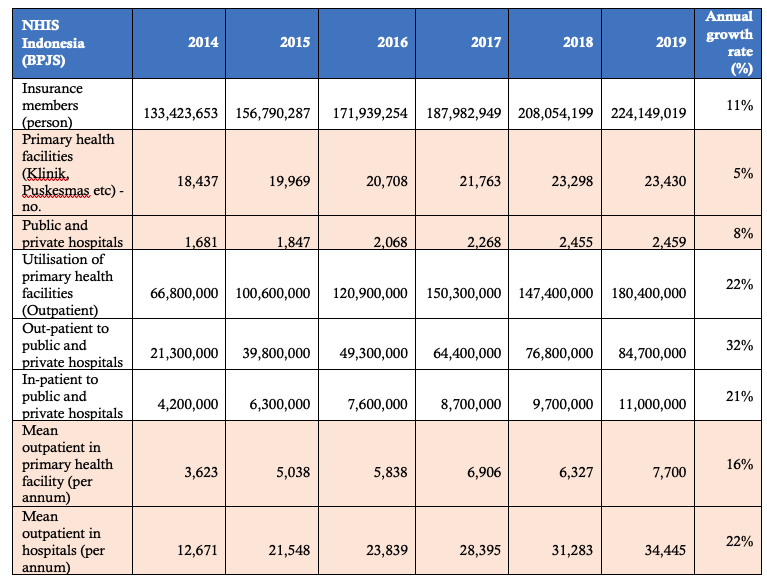
Indonesia commenced the National Health Insurance System (NHIS) or BPJS Kesehatan in 2014. Before the NHIS, health insurance for the public was fragmented and could not effectively reach the most vulnerable people i.e., people below the poverty line. In 2019, the system covered almost 224 million people or around 85 per cent of the Indonesian population. Over the five years since the implementation (2014-2019), the following, as shown in Table 1, were noted:
- Total outpatient services in the primary health facilities such as GP clinics, community health networks (Puskesmas) increased almost three-fold from 67 million in 2014 to 180 million services in 2019 or growing at 22 per cent per year.
- Total outpatient services in hospitals, both in public and private hospitals covered by the NHIS, grew at an even higher rate than the primary health facilities from 21 million in 2014 to 85 million services in 2019 or 32 per cent annual growth rate.
- Average outpatient services in the primary health facilities such as Puskesmas in 2014 doubled to 7,700 services or 21 services per day in 2019.
- Average outpatient services in hospitals in 2019 almost tripled that of 2014, increased to 34,445 services or 94 services per day.
- However, the growth of health infrastructure does not align with the growth of demand for health services. The growth rates primary health facilities and hospitals are only 5% and 8% respectively.
Table 1. Key statistics in Indonesia’s NHIS (BPJS)
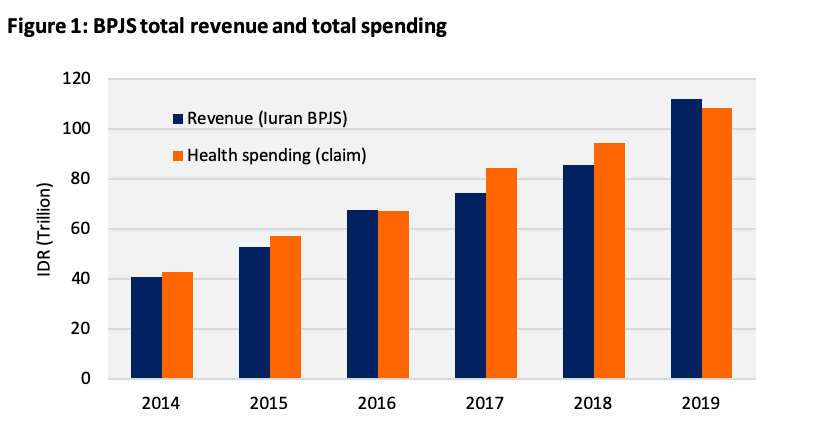
In terms of funding, the NHIS faced the issue of financial sustainability as the system underwent budget deficit in its early implementation years. However, according to its latest report in 2019, it achieved budget surplus, which could reflect substantial efficiencies (Figure 1.)
There are some challenges in the scheme as follow:
- Inadequate health infrastructures. Primarily due to low-quality infrastructures in primary health facilities, which include insufficient drug and medical supplies, mistargeting, and lack of health information system.
- Low health workers per population ratio and health workers distribution. Data from 2004-2015 show that the ratio remains unchanged per 100 thousand population with only 16 general practitioners (GPs), 88 nurses, and 44 midwives.
- Payment system. The current system applies two mechanism: first, is capitation and advanced payments for primary health facilities; and second is case-based groups (CBGs) for hospitals, which is based on approved tariffs for medical services.
How to improve the system
Health infrastructures, health workers ratio per 100 thousand population and health workers distribution require the commitment from Government and will take time. However, improving the system to standardised medical services, drug administration and payment system can be developed in timely manner for the sustainability of Indonesia’s NHIS.
WHAT WE OFFER
- Our experts are experienced in the healthcare industry best practice. The foundation of Universal Healthcare Cover (UHC) is transparency in medical services and pharmaceutical costs. Although the Indonesian Government has implemented the e-catalogue to manage procurement of drugs and medical supply that are cost-effective; one essential improvement is needed in this space. That is, providing information on cost of medical services and drugs to the public. In Australia, such publicly available information, Medicare Benefit Schedule (MBS) and Pharmaceutical Benefit Schedule (PBS), can be accessed online.
- We can assist in developing best practice payment system. The current system of case-based groups (CBGs) is deemed to be inequitable. The CBGs tariff focused on differentiating fees according the hospital classification . This results in higher fees for larger and better-quality hospital than small hospitals for the same medical services. The system is cumbersome and financially unsustainable. The best practice is to apply payment based on activity-based funding (ABF). Many countries apply the ABF, which takes the average from each patient episode such as inpatient admission, emergency department (ED) presentation, outpatient as well as a range of rehabilitation and mental health service. The ABF system provides measurable value for the public investment in healthcare system, promotes transparency of the funding, and ensures the sustainability of the insurance funding.
